Introduction
OK. I think we’ll get going. Welcome, everyone. Thank you for those of you who have introduced yourselves through the Chat there. We are really excited for our fourth and final webinar in our Kitchen Conversations series on telehealth. Thank you for joining us. Some of you have been here all along the way, which is fantastic.
So we’ll get started here. Today, we are thrilled to have Cindy Harrison joining us. Cindy is a speech language pathologist here where I am in Ontario, and she will be introducing herself in just a few minutes. I just want to run through a couple of housekeeping things first.
So first of all, this will be a recorded session. We will be putting all of these webinars from the series up on our website. Two, actually three of them are currently up there right now. And this will be up just as soon as we get it closed captioned. And you can find that on our website at exceptionallives.org. Your audio will be muted during the session, just so we can get through everything we need to get through in this 30 minutes.
And there will be a question and answer section at the end, about 10 minutes. So if you can look on the Menu bar there, where you saw the Chat function, there’s also a Q&A function. So if you click on that, it will open up your Q&A box. And go ahead and put any questions you have for Cindy in that box.
And if you can think of them now or as she’s going, just put them in there, and we’ll collect them and be sure she has those at the end to answer questions. And if we don’t get to all the questions, Cindy has generously offered her email so we can follow up with you and answer your questions there.
And you’ve already used the Chat function, and so again, it’s on that Menu bar. If you want to chat with your fellow participants during the webinar, feel free to go ahead and do that. Just be sure to change the To, where it says To All Panelists Attendees, not just the panelists.
So just a bit about Exceptional Lives, because we have talked about that in the past. We are a free resource available online. We have a lot of state-specific information for the states of Massachusetts and Louisiana. But we also have a national component.
And basically, we are finding the information that you are looking for to help with disability-related processes, and we try really hard to make it easy to understand so that you can take the information you need to move forward and help your child and your family. So this webinar series is part of that, and we’re really happy to be here with you.
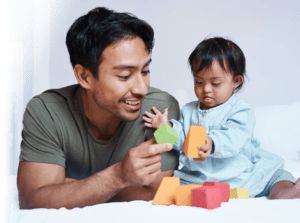
So why did we start this series? This is one of my guys on his first speech teletherapy session at the beginning of this pandemic. I am happy to say that it has increased in time. So this session you’re looking at was about a minute worth of session but he’s been doing great over the time, and the speech language therapist has been fantastic to just move with him.
So the questions that we had ourselves and that we heard from you are, how does this work? What does it look like? Is this an option?
And how do we get a child to sit still who’s not really sitting still to look at a computer screen? So Cindy is here to answer those questions and more. So we will answer this quick poll here and then move forward.
So we’re just curious about how it’s going for you at this point. It’s been a number of weeks now. So we’ve all had our ups and downs, I think. So we’ll just give this a second. Depends on the day. I really get that. That feels right. The struggle is real. It really depends on the day. So Cindy, with that, I will hand it over to you.
Presentation
Thanks, Julie. Hi, everybody. I wanted to thank you for taking the time to spend a half hour with me. This will be a fairly quick webinar. And so, like Julie said, I have left my email address at the end of this. So if I don’t get to your questions or if you have more, please feel free to reach out to me.
So I am a speech and language pathologist in Ottawa, Canada. And I am the parent to two amazing young adults. One of my kids is on the autism spectrum [Louisiana Autism Guide/Massachusetts Autism Guide]. So I wear a couple of different hats. I come at this as a parent of a child who’s now a young adult with special needs and also a speech language pathologist.
My area of expertise is working with children with autism spectrum disorder, developmental disabilities, and global develpmental delays. So I’m thrilled to be here. And these are definitely unprecedented times. So you can see some of these statistics here– 48 states, and I don’t know what it is in Canada, but I think it’s a fairly similar percentage– have ordered or recommended that schools do not reopen this academic year. Will schools be safe in the fall? Next slide, please.
So how do we adapt? And one of the questions we ask, is virtual therapy for us? And as clinicians and practitioners we’re asking, is this something that I can do? Is this something that I want to do? Is this something that I’m going to be good at? How do I protect the privacy of the information of my client’s personal health information?
Lots and lots of questions. And I think that one of the things that happened was that we had to pivot so quickly that really we didn’t have as much time as we would normally have had to be able to approach this in a very thoughtful, systematic kind of way. Next slide, please.
So how does virtual speech therapy work? In my opinion, if your child’s speech and language therapy was playful in person, it needs to be playful virtually. And I think one of the things that kind of paralyzes us as clinicians is we think, well, I’m going to be sitting static in front of a computer screen, interacting with my client through a computer screen, and there’s sort of that feeling of almost like an artificial or a tightness.
And so virtual therapy doesn’t have to take place with the child sitting at a desk. And I’ll talk about that in a minute. It can happen in the kitchen. It can happen in the backyard. It can happen in the playroom. I sort of sound like Dr. Seuss there. It can happen anywhere. Next slide, please.
So when we made the pivot, we decided quite quickly to pivot into virtual therapy. The clinic that I am a founder of, we had to lay off all of our staff when we closed. And in Canada, the Canadian government also announced quite shortly thereafter that they would pay 75% of the wages of clinicians.
And so we thought there are all kinds of families out there that need our help. We brought all of our staff back at full salary and benefits, paid the additional 25%, and then offered free services, free virtual services, for families until we could make the pivot and start offering these services to our clients.
So what I started to do was I would send the parents a quick email, just saying we’ve got a virtual session tomorrow. I was thinking that we might want to have it set up in the kitchen. What are your thoughts? Sometimes we would set it up outside.
All you need is, as you all know, is a cell phone or some kind of electronic tool that will help you to engage in a video conferencing space. Of course, we have to take a look at the programs that we use to make sure that they are– sorry. Can we just go back, Julie? I think we skipped ahead by accident there. Thank you. And so again– sorry, next slide, please.
So some sessions– being really honest– some sessions are great some not so much. And what I came to is I just needed to say to the parents, you know, it’s partly– it could be me. It could be me not really being sure about how to engage a child that doesn’t want to really be engaged in that technology.
It could be the child just saying this is not on for me today. And so I just said to parents, if the session is 15 minutes, I’ll bill you for 15 minutes. If it’s 45 minutes, I’ll bill you for 45 minutes. But we just have to let this be and roll with it, because it will be what it will be. Next slide, please.
So some of the advantages to virtual therapy, and this is something that has really been a silver lining moment for me. I see a number of very young children, so 6 months to 24 months is the bulk of my caseload right now, even though I do see children that are older.
And what I have found with that population is the family is saying to me, I do not have to put Johnny in the car, drive him 40 minutes through traffic to see you, put him back in the car, and drive him 40 minutes home. So it takes place in the home environment, in the child’s natural environment.
It’s been great for me, because I can see the setup of the environment. It can give me ideas to suggest to parents on what they can work on. So that travel piece has been quite big. The other piece that I have loved is that parents, grandparents, caregivers, family members can participate in the sessions. Now, with the COVID lockdown, we didn’t tend to have a lot of extended family in the sessions. But we certainly had siblings. Next slide, please.
So some of the challenges. When you have a family working at home, where both parents may be working in the home, where there may be more than one child– a number of my clients have more than one child with special needs– it can be really overwhelming.
The other piece is that very young children, in my opinion, require a therapy buddy, somebody that will help them navigate and to be their sidecar, their person that helps them navigate through the therapy session. Older children don’t, but many younger children or most very young children do. The sessions are less predictable and the environment is a little more difficult to control. Next slide, please.
I talk a lot with parents about the loss of control with COVID. So I think it’s really important, especially when children and youth have challenges communicating that they have some agency or control over what is happening. So much of their routines are out of sync. The people that they’re used to seeing aren’t there. The organizations, the schools that they go to, the preschools they go to, they can’t go to right now. And I think most importantly, everybody is in close quarters. Next slide, please.
So I talk to parents a lot about, if your child is verbal, that’s one thing, but if your child’s not verbal, let’s make sure that they’ve got a way to tell us. Whether that’s through gestural communication or through augmentative communication, to say I need some time alone.
It’s too loud. Please go away. Please be quiet. Come here. Can I have a hug? Don’t. No. I’m done. No more. Please don’t touch me.
And it’s just so important that the child feels like they have the agency and control to have a little bit of quiet time to themselves — where they can just be on their own and recharge in their quiet. They’re the same. I think of kids the same as adults. The extroverts tend to recharge with people around them, but for introverts, I think COVID has been very challenging. Next slide, please.
Communication and anxiety. One thing that a lot of my clients are saying to me is that they’re seeing regression in their children. And I think this is absolutely normal and to a certain extent expected. None of us, nobody on this call, communicates at our highest level when we’re not feeling well, when we’re anxious, or when we’re disregulated. So the question becomes, how can I support my child during COVID-19, especially if that child is having speech and language and communication challenges? Next slide, please.
One of the things that I really like and I’m suggesting to families is that they do a photo journal. It can be something as simple as just taking your cell phone and driving, taking the route that you would drive to preschool or to school and snapping photos along the way. Snap a photo of the school and the door the child typically goes in.
Ask your child’s teachers and caregivers if they can send a picture or meet them on a Zoom call and you can take a picture of them. Because one of the things that my clients are telling me a lot is that their child is just really missing the sense of routine, this sense of predictability, and those important relationships, both therapeutic relationships and otherwise.
So one of the things I’m recommending to families is that in quiet times, you can sit with the photo journal, whether it sits on your phone or you print it off, and just really talk with your child about there is Miss Smith.
Hopefully you’ll see her on a Zoom call next week or there are Nana and Papa, and maybe we’ll get to see Nana and Papa soon. Those sorts of things so that the child can feel that anchor to the things that are important in their life. Next slide, please.
It’s really important to give yourself permission to just abandon the agenda, to say this isn’t going to work for me today. We are going to have a therapy-free day. One of the families I work with say it’s a therapy-free zone. And you can just prioritize the relationship and be together. And I think it’s really important. One of the things I say to the families that I see is, be gentle with your expectations of yourself and your expectations of your child.
The other thing I talk a lot about, the families that I work with is, feel free to revisit comforting routines. We’ve been doing that in our family with a 25 and a 23-year-old. So we have all four of us in our home right now. And three of us are actually working from home.
And we actually sat down and said, let’s think about the favorite movies that we used to watch together. One of them was Home Alone. Every time I watch it, I think this was really a favorite movie? But it was a very comforting routine. So sometimes screen time isn’t all that bad in times of COVID. Next slide, please.
So it’s important to remember that even if you aren’t participating in structured activities, you’re still helping your child. So my suggestion would be to talk to your speech language pathologist about ways to help meet your child’s speech and language goals by weaving them into everyday activities. And probably most of you are doing this already, but it becomes more and more important in times of COVID.
Be creative and find what works for you. I have some families where their kids are not participating in any virtual therapy, but the parents are meeting me in a Zoom Room, and we’re working on virtual coaching sessions, problem solving together, coming up with ideas to weave the speech and language goals into favorite activities. Next slide, please.
So I wanted to just thank you all for– I kind of feel like I zoomed through this in the Zoom Room– to thank you for spending time with me, and I think these are very trying times with COVID-19 and the pressing need to stand up and speak out about racism because of so much of what’s going on in our world right now. It’s really important to remember to be kind to ourselves and to practice self-care.
So I have really raced through this, because we want to have you on your way in a half an hour. We know that this is a challenging time, and we don’t want to take up too much of your time. So I will open this up to questions now. And if I miss anything, my email is on the screen. Please do email me.
And for the providers that are on the call, if you have questions about– and I’ll help you as much as I can– about how we made the decisions to select the technology that we selected, to make sure that it was HIPAA compliant or if you have questions about some therapy strategies, whether they be boom cards or virtual libraries. Get Epic is one of them. If you have any questions like that, feel free. Parents, also reach out to me and caregivers if you have questions that I can’t answer in the next few minutes.
Questions & Answers
Thank you, Cindy. That was wonderful. OK. So our first question, which I’m happy to have gotten this question. This is in our house an issue right now. How can I ask my therapist for help with communication between my kids in regard to sibling rivalry?
Yeah. That is a really good question. And I think that virtual care, if your provider is happy– or is comfortable with it, I’m sorry– if your provider is comfortable, you can actually have a couple of– you can have your kids join in together so that your therapist can see what’s going on and can give you some suggestions and ideas.
The other thing that I have done is I’ve negotiated with parents to have maybe 5 minutes or 10 minutes at the end of the session where the kids come in, and they join the session. We do something together that’s fun. That’s also an option.
But I think that some of the downsides of not addressing these very real issues can be quite problematic, because the other kids see that Jimmy is having fun with a speech therapist, and why can’t I join in? And so almost all of the virtual sessions that I’m doing either have siblings in for a lot of the session or at least for part of it.
Great. OK. Next question here. How to start work with a 3-year-old who does not yet say a single word.
I actually have a full– I would say two days full of kids who are preverbal. And all of them are under 3. And my answer to that, and this is just the way that I practice, is I work in a parent-mediated model. So the parent or parents, depending on whether or not both parents are caregivers, can join, are in the session with me. And we play.
So basically, what I will say to them is, tell me the one thing that you do together that brings you joy. And that’s where we start. If it’s a chase and tickle game, then that’s what we do. And I coach from the other side of the screen. If it’s one little guy loves water play. So we go into the kitchen. So I think that the big key there is– so this is sort of a long answer.
This is a really good question, because we know and research plays this out that most of the precursors for appropriate language production are actually nonverbal. The gestural communication, the child’s ability to engage with their play partners, the ability to have a conversation without words. So the baby that reaches her hands up to say I want to be picked up and then mommy gets distracted and goes to help another child and the baby goes, ooh.
And mommy turns around and says, oh, you want up. So that’s a really good question. So much of the work that I do is actually preverbal, because we know from research and we know from clinical practice that those preverbal skills, what happens before the first words, are very, very important. That’s a great question.
Yeah. That’s great. OK. So moving to the next one. Do you find that telehealth changes the way parents interact with their kids and perhaps helps them learn the techniques you’re working on?
Absolutely. And I find I work in a parent-mediated model even when we’re face to face with the little guys, because I call it the co-quarterback model of therapy. I have a lot of knowledge in speech and language, but the parent is the expert on their child. So when we put our heads together, then we can come up with an appropriate plan.
So the rule in my clinic for myself and our staff is that parents are invited into every session. And in fact, if they can make it, that’s the way we prefer to work. So I think that– sorry, I just realized I kind of forgot the question. I think I wavered. Can you repeat it again, please?
Yes. No, you were there. Do you find that telehealth changes the way parents interact with their kids and maybe helps them to learn the technique?
So what parents are saying to me is, there is a sense of comfort. Once you get over the awkwardness of knowing that there’s a camera in the space, there’s a sense of comfort in being in their own environment and a sense of comfort and going, oh, OK. This is how I can use this toy, and this is how I can change the way that I’m relating when we’re in the kitchen and he’s helping me do the dishes or when we’re baking. So I do.
And interestingly enough, the silver lining for me is that post-COVID, I am going to continue doing at least one, possibly two days virtually. And a lot of clients are saying to me, this is working for us. We get to be a vital part. In fact, we have to be a part of therapy. And it’s in our own home. So it’s going to continue post-COVID, which I’m very happy about.
We’ve heard that from I think all of our presenters so far. So that’s definitely a common theme. What would you do with a child who’s just refusing to participate in telehealth sessions?
I wouldn’t push it. I would say, there is a reason that the child is refusing. And so at that point, what I would say to the parents is, I’m happy to do some virtual coaching with you. I’m also happy to come back and try it again in a week or two. If it doesn’t work, we can try it again. If it doesn’t work, then let’s look at a face-to-face option that will work better for your child.
There’s so much about COVID that just makes this feel so out of control, that I think the last thing that you want to do– my concern would be that I would be impairing or damaging the therapeutic relationship with the child by asking the parent to insist and also the the attachment relationship between the child and the parent, if the parent felt they needed to force it. So I don’t. I just don’t recommend forcing it.
OK. So you talked a bit about regression. So should kiddos be asked formally or informally to determine new needs if there has been regression during online learning?
So yes and no. I think one of the things that I say to parents is– and this is only my opinion. I don’t love the testing and testing and more testing. I do think that diagnostic therapy is helpful so I can be a good clinical observer.
And what I say to parents is, regressions like this are rarely permanent. So what the child is telling us is that for some reason they’re under a lot of stress right now. We can probably think about 100 reasons that might have caused that.
So let’s meet them where they are, and let’s focus on what they’re giving us. And we’ll come up with some strategies around that. Let’s tweak the therapeutic approach, but I don’t think there needs to be a formal reassessment, because it’s a temporary state. And interestingly enough, now that families are sort of hitting the rhythm and the stride of COVID, we’re seeing that regression starting to shift and change.
And some kids, the regression started to shift and change when their parents introduced a photo journal, where they could actually see the people that are important to them, see pictures of them, when they started doing Zoom calls with their early childhood educator or with their speech pathologist or their occupational therapy or their instructor therapist.
So I don’t think that there’s a need for formal evaluation. And a skilled clinician will be able to figure out where the child needs to go. And we’ve got the experts, the parent, to help us understand what’s going on as well.
I love how you described the photo journals and even the movies, the old meaningful movies as an anchor right now, because I think we’re all looking for that. And there is one bullet point where you said parents notice regression or something, and I thought, oh, that’s interestingly worded, because as a parent, there’s also moments of regression, where like stress and that kind of thing.
So I think that’s a big one right now. OK. So we have someone who’s saying, when my child is asking for something he needs, he pulls my hand but doesn’t try to speak. He doesn’t look at my eyes when I try to call his name or to say something.
So one of the things– there are two things there. And I don’t know your child. So this is a little bit difficult. So I’m going to do my best. One of the things that you would want to do is if you know, because you’re an intuitive parent– that question shows that you’re an intuitive parent– what your child wants, I would hold up the two choices. So cookies and something that you know he doesn’t want, broccoli, by your face and ask him which one.
He doesn’t need to speak, but he’s more likely to look at you if you’ve got the items right by your face. And then if he reaches up or if he makes a vocalization or a sound that’s enough for you to understand what he wants, then I would give it to him.
What we tend to do as parents is we are so adept at figuring out what our kids want that we just give it to them, and we lose that opportunity, not knowing– unknowingly– to get them to interact. So I would try that and see if that helps.
Great. OK. And we’re just going to wrap up here, Cindy. But we do have someone who’s asking you if you’re accepting new clients and can you share your information.
Yes, I am. And you can reach out to me at the email that you have, charrison@actlearningcenter.ca.
Great.
Thank you.
Conclusion
OK. So thank you so much, Cindy, for being here and for answering our questions and sharing this awesome information with us. To everybody who participated, thank you for being here, and we will get this up on our website as soon as possible so you can share or review.
You can fill out this quick poll here. And if you’re looking for more information, please check us out at exceptionallives.org. And we will be in touch soon through our newsletter or on social to keep you updated with what we’re working on next. Thanks a lot.
Thank you for having me.
Thanks, Cindy. Bye.
Bye.