Follow up questions
I can’t always understand my child and I feel terrible-Help!
Am I doing enough?
What strategies can I give my child to help her be understood?
Introduction
Welcome everyone. We’ll get started here because we do have a short 30 minutes time slot today. So we want to make sure to get everything in. So welcome to our third and final webinar Kitchen Conversation and our Summer series to learn about speech therapy during summer. So Cindy is here with us. We’re very happy to have Cindy with us again, to talk to us about speech and language therapy and how we can incorporate this into our summer days.
So just a couple of housekeeping things to remember. We are recording the session, so if you follow us on social media [Facebook/Instagram] or subscribe to our newsletter, we’ll be sending out a message when it’s available and up on our website with closed captioning. Your audio will be muted during the session but if you have questions, please share with us. So if you could pull up the Q&A icon there, click on the Q&A icon and a window will pop up. That’s where you can post your questions and we will keep track of those so that we have time reserved at the end, so we can answer all of those questions.
We also will be getting back to you with questions that go unanswered. So Cindy has graciously agreed to record herself answering those questions and we will post those on social media and make sure that you have access to those as well. Finally, the chat function– some of you have already used this to introduce yourselves. Thank you for doing that. The chat function will keep going the whole time. So if you have questions or if you have comments as we go, please feel free to share with the group.
So a bit about Exceptional Lives, we encourage you to please go to our website and poke around, see what speaks to you there. We provide disability information for free on our website and we do that through a few different formats. We have blogs [English/Spanish] and guides [Louisiana Guides/Massachusetts Guides] and a searchable resource directory [Louisiana Resource Directory/Massachusetts Resource Directory].
We also have some information that’s specific to the last few months during the pandemic. So being at home finding some resources that you could use at home as well, which is part of what we’re doing here with our webinar series. Thinking about integrating the therapies that we’re all accessing, how do we do that now that we’re at home?
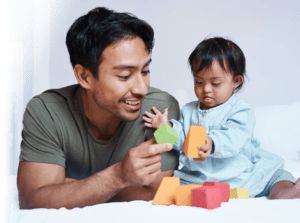
So with that, we will move– my name is Julie. I always forget to introduce myself there and this is my son here, who is receiving speech therapy but it looks very different in the summer. So I put this photo up because for our family, he is constantly moving in and out, he’s on his bike, he’s off his bike, we’re trying to get food in him. So how do we continue to think about our speech goals with a moving target the whole summer?
So that’s something that I’m thinking about and I know that a lot of parents have a lot of questions about how that works in their family. So this poll that you may have already answered, but how is speech therapy going for you this summer? If you could answer there then we’ll move on to Cindy. We’ll just give that a few minutes here.
OK. I love this. So it’s a range. In speech therapy and using strategies regularly. In speech therapy but that’s it’s. Not currently with a speech therapist and wanting to learn more about child speech and communication needs. And we also have providers. And some of us are providers and parents as well. So great. As we go, please feel free to share in the chat. And again, we will have your questions at the end. And Cindy, I will hand it over to you.
Presentation
Great, thank you. Hi, everybody. Thanks for spending this half hour with me and with the team at Exceptional Lives. My name is Cindy Harrison. I’m a speech and language pathologist in Ottawa, Canada. And so you’ll notice a few different spellings in my PowerPoint as we go along.
So today, I’m looking to talk to you about some tips and tricks to facilitate communication at home with your child. And I think that it’s well-known that there are many everyday opportunities to help your child develop communication. You can use these opportunities to turn them into teachable moments or learning opportunities.

I think it’s really important to think about the fact that with so many of us working at home or from home rather during COVID-19, the pressures on parents are significant. And I know that the clients in my practice are saying to me, we are just trying to get from 6 o’clock in the morning until 8 o’clock at night.
And many are feeling overwhelmed, some people are feeling a sense of guilt because they’re needing to fulfill the commitments of their job while having their kids at home. And I think it’s just really important, be kind to yourself. It’s a really difficult balance and anyone says if they’ve got it all figured out during these times, I think is probably not telling the truth.
So one of the things that you can do is make favorite items inaccessible. Sometimes our kids are very resourceful in getting what they want, and sometimes they’ll have the idea that they want something and they’ll just go and get it. So you may want to put your child’s favorite items up on a shelf or a counter that your child can’t reach.

Sometime with them, sometimes with younger kids, I will recommend to parents that they use double sided Velcro tape, and just stand like a Ziploc freezer bag, and put favorite toys in the Ziploc bag and then stick the Ziploc bag higher up on the wall where the child probably can’t reach. And this will encourage your child to reach, to point, to vocalize, to verbalize, to request their favorite items.
Create the need for help. So this is where you play a little dumb and you create the need for assistance. You can prompt your child and wait for them to respond. For children who are more verbal, you can model for them.
Create the need for assistance. You can hand your child a jar of bubbles with the top screwed on really tightly. you can hand them a juice cup but have the juice way up on top of the fridge. You can hand them their applesauce with no spoon. Those kinds of things will encourage them to use gestural communication or to use words to ask you to help them.
You can take advantage of everyday teachable moments. So ask your speech and language pathologist to identify target words or concepts for everyday activities that will help you to know what words to target.
So I think it’s always important to think about, for example, if the concept is in or out, your child is going to gain that concept much more quickly if you are standing between them and the door, and they have to express either through gestures or through vocalizations that they want out. Versus maybe looking at a picture of a girl walking outside the door and saying she’s going out. So the more you can make it relevant to the child’s environment, the more you can make it something that’s motivating for them, the better. So weave the target concepts that your speech and language pathologist identifies into everyday activities.
Choices. Lots and lots of choices. So you can offer your child something that you know he or she doesn’t like and then you can model, no yuck, et cetera. You can offer something you know they like along with something that they don’t like. So they might answer you with a gesture pointing, they might answer you with a vocalization ah to say that they want the cookie, or they might use a word approximation “use” for “juice” or they may use the word.
For children who don’t often look at you, try to hold the choices up near your face so that you can encourage them to look at you while they’re engaged in the interaction. You can give small portions. So you can give one French fry or a few sips of juice in a cup or a few pieces of pasta and then you can look at your child expectantly.
We’re very good as parents I think, at understanding and guessing what our child wants. And so if you’re a bit more purposeful about it and you give them just small portions of something they like, then they’ll have to indicate to you through gestures, through a word, through a word approximation that they want more. And that’s another way that you can get them to use their communication skills.
Modeling– You can interpret what your child is trying to say. So if your child says “use” instead of saying no, say “juice”, you acknowledge, yes, “juice”. And you can model the correct production. And you want to label what your child is trying to communicate. So if your child is going [grunting] you say “mad, so mad..” so that you’re helping them by modeling the word in the hopes that they will model that back to you at some point.

You can expand on what your child says, “mommy plane”, “huh? Yes the plane in the sky.” So you can expand on what they’re saying. If your child gives you a word approximation, you can model the word back correctly. Could avoid saying “no not use tell me juice” because that I’m sure your child will be thinking, if I could say juice, I would say juice. So it’s really important for you to interpret the meaning behind their utterances.
So this is quick. In closing, be kind to yourself and by weaving these tips and tricks into everyday life, you’ll be doing more than you think you are to help your child speech and language to develop.
You can feel free to reach out to me with any questions and I know we’re going to open it up now for questions. At charrison@actlearningcentre spelt the Canadian way, with a t-r-e on the end instead of t-e-r and I’ll be happy to respond to you. And like Julie said, I will also be happy to take any questions that I’m not able to get to today and record some answers for them, that will be made available to you on the social media page. So I’ll open it up for questions now.
Questions & Answers
Thanks Cindy. That was great. We do have a few questions here. So we can get started. First:
Q: It’s hard for people to understand my child under normal circumstances and even harder when he wears a mask, he’s getting really frustrated – SOS please.
A: Yeah. Poor guy. I really can understand that. And in answer to that question, we’re finding that a lot with the kids that we see not only are they struggling with the masks but they’re struggling with us wearing the masks. Because there’s so much that happens on our face in terms of gestural communication and facial expressions that gives meaning to communication.
The first thing I would suggest if you haven’t got one already is looking at the masks with the clear cut out, so that you can see the child’s mouth. You can wear that and your child can also wear that. I don’t have the– oh I don’t have the website, it’s right at the tip of my tongue but I can’t think of it.
There is a website, it’s based in the US and they’re making a mask that actually has been approved by the government of Canada– I don’t know if the FDA has approved it as safe to use because some of the masks, I think there were some questions about whether or not they were sufficiently safe to use as face coverings, but if you want to email me, I will send you that information happily.
In terms of your child not being able to be understood, I don’t know the age of your child so I’m hoping that this is an appropriate suggestion, but I would have the conversation with your child but you know it’s so difficult because people can’t see his mouth.
But I would also try and use as much as you can– speech pathologist call them “close” or they are really “fill in the blank”. If you can use “fill in the blank” and ask your child, depending again on his age, if he’s OK with you being a bit of an interpreter because people are having difficulty understanding him because of the mask. And if he’s OK with it, I would go ahead with that. You can also use the word fill in the blanks, “oh you are trying to tell her that you’re feeling”– and then he can fill in the blank.
Again, I don’t know the age of your child, so I don’t know if that’s developmentally appropriate or not but if your son is old enough, I would have that conversation with him so that you have a better understanding of how you can facilitate him being better understood. Definitely something we’re hearing a lot from families.
Great. And we can also post that link, when you find it Cindy, on our social media so we can share it with everybody, thank you.
OK.
Q: If you’re holding back toys or like giving only one French fry, how do you balance doing that and managing frustration?
A: That is such a great question. Because at the end of the day what is the most important to any parent is the relationship with their child. And we don’t want to put our kids in a situation where they’re thinking or they’re interpreting, mom you know what I want or dad you know what I want. Why won’t you give it to me, why are you playing clueless, pretending you don’t understand?
And so I think it has to be a balance. I’m a speech and language pathologist and I guess you could say I’m a content expert in communication, but you are the expert on your child. So I think I would try it a few times, and if your child is OK with it. So if your child goes when you hand them one French fry because they get that you’re being funny, then you can continue with that. If your child looks hurt or looks frustrated, then I would not, I would say like, “oh silly mommy I gave you one, do you want more?” And let them indicate yes or no.
I would never not accept. So let me back that up. I would always accept, we’ll frame it in the positive way. What your child does to tell you that they want more if it’s a oh, that’s OK, then you give them more. If it’s a more a word approximation then they get more.
So really it’s something that I would encourage you to use your knowledge of your child. But I would always err on the side of I’m giving up before you frustrate them. And if you do frustrate them, which I have done many times in my practice not meaning to, I will say, I’m sorry, I made you mad. And you can just own it and then move on. That’s a great question.
I really like how you’re always checking in with the child to see what their– is it OK if I do this? Or I’m sorry I made you– like you’re keeping that communication open to which I get is, sounds really respectful.
I think we need to. Because, we need to give our kids the agency to feel like they’re in control, and that they’re heard, and that they’re seen. And that’s what we all want, right?
Yes.
All right. I interrupted you.
No. That’s OK. OK, so the next one here.
Q: Suggestions for older kids like ages 5 to 7 to increase expressive language?
A: Yeah, that’s another good question. I hate to make a vague answer. It depends. So with an older child, if they’re highly verbal, some kids need help with formulation. They know what they want to say, they have an idea of what they want to say, but it’s very difficult to organize it. So with those kids, you can do a little bit of first then. So you can say, oh yes what do we do first? What do we do next?
With a child that’s a very visual learner, you can also have something that they can look at that might have a number one, a number two, a number three, a number four. So first we, then we– Just to help them organize their thoughts.
For an older child of 5 to 7 who is really struggling to get something out and sometimes kids will get excited and they’re trying to tell a story and it’s just not working, you can very calmly say, “oh you are really trying to tell me something, I really want to understand.”… “So you are telling me about– oh, I get it.”…”OK, this story is about when you and Ben went to the park, what did you do?” So you can ask some questions that help the child better formulate or organize what they want to say.
This is a bit difficult for me because I don’t know the comprehension level of your child, but if you want to email me and give me a bit more specifics, I’m happy to send you back some suggestions either on a videotaped answer or by email.
Great, thank you. OK. Let’s see the next one.
Q: When giving my 3-year-old choices or having things out of reach, how do I respond when she just whines, do I give it to her anyway?
A: Another great question. So again, you’re the expert on your 3-year-old. You do want to set it up so that you at least get something If you know what she wants, that you at least get something from her. So if you have something up high that she wants and she’s whining, I would get down beside her on her level and look up and then point say, “oh is that what you want?” And you can take a head nod, you can take her reaching up, you can take her going huh, you can take anything.
But I think that you should first try to stay in that place where there is a little bit of tension. Because your daughter’s probably a really smart little bunny and she knows what she wants, and she knows that if she whines, it’s likely that you’ll understand what she wants and give it to her.
In fairness to her, she could be whining because she knows that she knows the word and she knows what she wants but she can’t actually ask you. So giving her the benefit of the doubt, it could be that she’s legitimately frustrated. But I think you want to at least give it a little bit of a try to see if you can get something from her. Even if it’s subtle, you’ll accept that and then immediately give her what she would like.
Great. OK.
Q: Could you please discuss positive ways to correct speech mistakes?
A: Absolutely. So I think the best way is modeling. And I think that the thing that I always think about and encourage parents to think about is even though we want, I want my job as a speech pathologist is to help with correct production and that’s certainly your job, that if the child could produce it correctly, they would. And it might be– for the child I’ll just use the example of a list. For a child that wants to say snake and says “nake”, it could be that with some support and scaffolding, they actually can produce the word snake. And so then you would want to model for them, “yes s- nake.”
It depends again on your relationship with your child. Because some kids are very much impacted by feeling that they’re being corrected. And they can get defensive, they can get sad, they can feel badly. Other kids are totally cool with being corrected.
So it depends also on your knowledge of your child. The best thing that you can do is give them back an appropriate model. The only thing that’s different there is I think you can negotiate with your child depending on their age, to say OK, for 15 minutes before dinner, every time you say s instead of s, I get to correct you. And you can set it up as a little bit of a game. So it’s almost like your own speech therapy session with your child but outside of that time that you negotiate, model the word back and then I would leave it alone.
OK. That’s great. That’s really helpful for me. That was not my question but I appreciate it.
Q: How do we get a child adjusted to wear a mask and keep it on? I’m really worried about school for my 7-year-old.
A: Yeah. I’m a parent of a child, well he’s a young adult now. And I’m very worried about that as well. He’s on the autism spectrum and has a great deal of sensitivity. I have a lot of kids on my caseload that can’t stand things behind their ears, they can’t stand things on their face, and it’s very real for them. So the best thing I can think about is if you can really try different models of mask.
So we have found with our son, they’re the surgical level disposable masks and they’ve got a really soft and long elastic. So he could put that on behind his ears and it didn’t bother him. There’s another little guy on my case, so it bothered him when it was loosen, it bothered him, it itched him, so we found a mask that had wider elastic that was a little tighter to his head. So I would try to find a mask that he can tolerate.
The other thing you can think about and this is going to depend, you may want to speak to somebody in the medical officer of health office, the other thing we have found is that some kids will wear baseball caps with face shields. You just have to be careful about the fact that the face shield extends back beyond their ear and down below their chin. So you can try that as well. But I can assure you that it’s an issue that parents are dealing with right across case loads, across North America and probably across the world. It’s really tough for some kids.
Yes. Yeah. OK.
Q: Cindy can you speak a little bit to Apraxia and those children that are more significantly impacted with ASD. Our son is non-verbal, although able to do some approximation. I feel like there is some Apraxia there but speech therapy says he has limited output and unable to diagnose.
A: OK. So without knowing your son and I don’t mean to contradict anybody, I’m just basing this off of a question. My attitude when a parent says I think there’s some dyspraxia there is always to say you’re the expert on your son. So I am going to assume that you know your son, you’re talking about what you were thinking and my assumption would be OK. Then let’s take a look at that.
I think you’re probably right. A number of kids who are nonverbal it does end up being the motor planning, that is the problem for them. And it can occur at the level of ideation. So your son has a rich inner world and it’s got to be so frustrating for him and for you that he can’t show you what is going on in that inner world.
And so I would want to know– I would immediately consult an occupational therapist, who looks at praxis in the whole body whereas, I would look as a speech language pathologist, I would look at praxis for the articulators Because sometimes we find that through collaboration with occupational therapists, we can deal with the motor planning if we deal with the praxis in a whole body way.
The other question I would be asking is, is somebody looking at augmented of and alternative communication for your son? And if not, they should be. But that doesn’t mean that you should give up on really addressing the praxis. Some kids with severe praxis do go on to be verbal, some kids go on to be more reliant or to use a CSV as their method of communication. But I always listen to parents and assume that what they’re seeing and what they’re telling me is what is.
Conclusion
Great. Cindy, I think we’re going to close here, we’re getting to the end of our time. It always goes very quickly. So if everybody– thank you so much for being here. And if you could just fill out this quick poll for us to help us as we continue to plan future webinars, we’ll let you know about that. So again, we will let you know. Check your inbox or social media. We’ll let you know when these are up online closed captions. Cindy, thank you again for being here. It’s very helpful.
Thank you for having me.
And thank you everyone for participating. So we’ll see you next time.
Take care everybody.