Click to Read Transcript
[Christina Kozik] At this time, I’m gonna hand it over to Anne and Kim.
- Thank you so much. So I am Anne, I am a 57-year old White woman with brown hair with a little bit of gray that needs to be covered quickly. And I am in a black polo, actually the matching shirt to Kim Haynes ’cause they’re our uniform shirts for McMains Children’s Developmental Center.
- And I am Kim Haynes. I am a 54-year, 53-year old, boy, man jumping up there, 53-year old, White woman with shoulder length, black hair and wearing the same shirt as Anne. All right, we are trying to, have you turned over control? Okay.
[Anne Hindrichs] All right, well then we will get started. So welcome, we’re excited to be here today, talking about therapies and accommodations, and unique to see that so many of you have children that are already in services, or I guess, the pros with us that are Individuals with Disabilities Education Act, which actually was a law that had been from, back all the way from 1975, which was the Education for All. And what it did was set up that all children could receive a free, appropriate public education along with the services that were needed and special ed services and whatever else to help that child. So for many of you who have been under EarlySteps in Louisiana, which has different names in other States, which might be a ChildNet, ChildSearch, Early Intervention Programs, was the Part C part of that law. And so now that your child is exiting out of that, they’ll would be gonna the Part B section of it, which is for children ages three, all the way up to 22, which then provide services within the school system. It is not budging, but I’ll keep going while we move it. Christina, can you turn the, there we go.
So first off, what is the difference between School-based Therapy and then the Outpatient or Clinic-based? For part C, for the EarlySteps, much of that, since children are not in school yet, the therapy has been done within the daycare center, home, whatever the best place for the child, and then as the child enters school, most of their days are spent at school, most of their time. So therefore School-based Therapy is then offered. And then we have, which we’ll talk about in a minute, the Clinic-based side.
School-based Therapy
So School-based Therapy is considered a related service. It is an educationally-based service, meaning that there are special services that come out of that direct services, such as Adaptive Physical Ed, which is APE or Assistive Technology. But it’s also based on whatever’s going to be more rehab based and it’s everything outside of that, community, in the home, even playing T-ball, but School-based is, How does my child succeed in school?
So some of the programs that are offered, services, Occupational Therapy, which again, we know are fine motor skills. We know that they’re the adaptive daily living skills. And when you get from school system now, you’re looking at, How does my child hold his pencil? How does my child organize the paper? How does my child pick up toys in the classroom, if it’s a preschool setting? Physical therapy then will look at, How does the child get from the classroom to the bathroom, from the classroom to the cafeteria? Do they need a walker? Do they need a wheelchair? Within the classroom, do they need other adapted equipment such as a stander? Speech and Language Therapy kind of crosses over both to where it looks at your language, can be a small group, can also be following directions of the classroom. It can be comprehension, but you’ll also see some crossover with that and with Clinic-based.
Orientation and Mobility for someone, this is strictly for children who have visual impairments or blindness, there’s someone, usually on vision therapy, a resource teacher who will come in and help that child, making sure that papers are adapted to the correct size so that child can see the same worksheet or the work that’s on the board. School Psychological Services, which then looks at the IQ testing, being able to qualify a child for services. It can also be working on behaviors. School Social Work Services, which looks at a social history, getting with you and finding out information about your child to put forth in what’s called the 1508 Evaluation. And then also School Health Services and School Nursing Services, which are basically set up if your child has seizures, that there may be a nurse on that campus, school campus, who’s able to help and be available if your child does have a seizure. It would also be someone with the health services that will help coordinate chronic care with a child. Making sure that all of the services are being brought in that’s needed. And of course, these are all put together in what would be called the Individualized Educational Plan, which is now the IEP, which before that, which everyone would recognize as the IFSP, which would be the Individualized Family Service Plan. So now it will change to that.
Outpatients or Clinic-based Therapy
So now Outpatients or Clinic-based Therapy. These are based on a medical model. So the therapies that are gonna be provided are gonna help your child succeed in the home, the community, and in other environments. Might even be just to help them, your child has a disability and he wants to play T-ball. That’s something that a therapist could actually help you with on figuring out how to adapt that and make it to where your child could participate. Occupational Therapy on this now goes, all of these are gonna go a little bit wider than what School-based would be. So it could be dressing, being able to button their shirt, being able to learn to tie a shoe. It can be organizing, again, the workbook page, or writing a story successful. Speech and Language Therapy, the same kind of thing that we talked about with school. The School-based Therapy for Speech and Language and Clinic-based, sometimes you will find can be very similar goals. Whereas some of the others may not be, those two probably are the closest. Management, helping you find the resources that you need within a community, but case management, social work can also be a parent support group, social skill groups, and as well as helping with parenting, parent training. And then psychological, similar to that as well, doing IQ testing, but also can help with parent training, can help with behavior management that would be needed. So the other big difference between these two things is that School-based Therapy is based on, it’s funded by Federal Funds. It was backed, the whole idea, the law was backed through Federal monies that came through. And so it is a free and public education, Free Appropriate Public Education for your child. Therefore you get those services at no cost to you. Since it is School-based again, it’s provided within the school, but Medicaid can be charged. It’s just no out-of-pocket expense to you. Outpatient or Clinic-based, rehab wise is going to be funded through Commercial Insurance, where you may have a co-pay to pay, or a 70, 30% kind of trading. Medicaid, that would also cover it, or it could be a sliding scale or just straight out-of-pocket if none of those will cover it. The important thing to remember is that a child can get both. They can get School-based Therapy, as well as Clinic-based Therapy. A child may qualify for a Clinic-based Therapy and not for School-based Therapy if the therapy that is needed is not part of helping them achieve in school.
[Kim Haynes] So how do I get therapy for my child? If you’re seeking services through the school and your child is not in school already, contact Pupil Appraisal and tell them what your concerns are, and then they will walk you through the process. If your child is already in school, start that conversation with your child’s teacher, that child’s teacher will then bring it to a committee called a School Building Level Committee, and they will meet along with you, and they may start off with just making, some general accommodations in the class, to make your child be successful. If that doesn’t work, then they may decide to do a full evaluation in the areas of concern. And then after looking at those evaluations, if your child qualifies for services, then they will, with you, as part of the team, develop the Individual Education Plan, that IEP, that will list all the goals in the areas that your child needs help in. If you are seeking services from an outpatient or Clinic-based facility, then you’ll need to get a referral from your child’s doctor and then contact the clinic, which will then set up the evaluations. And then once the evaluations are complete, that clinic will get with you and let you know the services that your child does qualify for and develop what, in Clinic-based is called a Plan of Care. And that will look at the goals that you’re wanting and the therapists are needing to accomplish for your child.
So what are some accommodations that may be provided for your child? So again, School-based Therapy, accommodations are geared to what will help your child be successful in that setting. And so they are based on helping that child succeed in the school setting. Now, these are just some examples like preferential seating, but preferential seating doesn’t necessarily mean sitting next to the teacher’s desk or in the front of class, because some teachers talk and walk around the room as they’re talking to the class. So in that situation, preferential seating may be in the middle of the classroom so that you are always near the teacher while she is talking or lecturing. It could mean not sitting next to the window that looks out to the playground. It could mean, if your child is easily distracted, not sitting by the door that is open to the hallway so that your child can see those things. So preferential seating means different things for different kids and that’s where the Individualized Education Plan comes into play for your child.
Writing aids your child’s goal is to learn to write their name or to write a sentence. So it could be something as easy as a pencil grip to help them write legibly, or it could be something as complex, if your child is just not successful using pen and paper, using a computer to help them get that information out that they need to get out. So these accommodations, again, are just tools to help your child become successful in that setting. It may be a peer buddy, somebody to help your child get from class to class, or maybe to take notes or just to be a friend and learn those social cues and help at recess and in the social settings. Picture schedules are always a nice accommodation if your child has trouble transitioning from one place to another. And so with a picture schedule, you can have a picture of reading class, then math class and then lunch. And so that you can talk about, Okay, now we’re finished with reading, and you remove that picture. Now, it’s time to move on to math. And helping that child understand what transitions are coming and helping them prepare instead of it just happening when the bell rings. Some children are very sensitive to noise. And so noise canceling headphones, especially while they’re trying to do seat work or quiet work may be a help for your child. And then simple communication devices. If some children have difficulty speaking or their speech is very hard to understand, or not speaking at all, simple communication devices to help them not only speak, but become interactive and part of that classroom setting. So those are some accommodations that can happen at the school level. So now let’s look at the Clinic-based, there we go.
So what are some accommodations that may be helpful or are started in Outpatient or Clinic-based? So it could include all of the same things that we just talked about, except for the preferential seating, because usually Outpatient or Clinic-based is one-on-one therapy. But the accommodations go again a little bit farther because it’s based on not only making the child as independent as possible in school, but in the community and at home. And so writing aids again and picture schedules and noise canceling headphones, but , maybe your child can order their food themselves using a communication device. Or use a picture schedule to actually place that order at McDonald’s. Or if you go to the playground, how will your child let you know what they want? Do they wanna swing first? Do they wanna go on the merry-go-round? So you can use a picture schedule, you could use a communication device. And so again, it’s geared, the Clinic-based has a broader area that they cover than just the school system. Mobility aids, again, in the school system, you’re looking at getting from class to class or from class to the cafeteria to where you may look, in Clinic-based on how do you get around the park? How do you get from inside to outside? How do you go down the street and visit the neighbor and what things are accommodations, what tools will help your child, excuse me, will help your child be successful in that situation? Yeah, there we go.
So when working with your therapist, it doesn’t matter if you’re School-based or Clinic-based. When you work with your child’s therapist, you are a very, very important part of the team. You know your child better than anybody else. You see what your child does day to day. Practice good and open communication. Tell your therapist all the things that you are seeing, what your concerns are, what your child can and cannot do. Share your goals with your therapist. When an evaluation is done, it’s based on the developmental milestones, but you may have a goal that is more functional and personal to you, like saying hello to grandma, or being able to talk on the phone or video chat with grandma and grandpa. So things that are important to your family are very functional and could be part of what you’re looking for, for your child with a therapist. Now a goal like that might be better suited for a Clinic-based, as opposed to School-based, but you could continue to work on the communication. Ask questions, if you don’t understand what your therapist is doing or trying to achieve, ask questions, there’s no problem at all. That’s how you learn and you become part of the therapy and know.
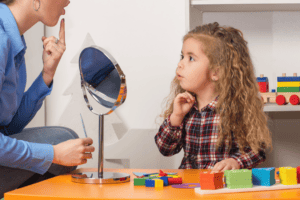
For example, if the occupational therapist is working with your child in stringing beads, you can say, Hey, what does stringing beads have to do with anything? At that point your therapist may explain that stringing beads is working on what’s called a pincer grasp, using those fingers to pick up food, eventually, or to hold the zipper so that they can dress themselves. And so that all of their activities build towards bigger goals, so ask questions. Enter into your routines, but therapists are always working off the evidence-based practices. And so be willing to try new things, to see if they change or help your child in any way. And again, if you’re not understanding or need more clarification, you can ask for a meeting. If you need more time than just a few minutes alone with a therapist to talk and practice, ask for a meeting, sit down and again, ask the team, whatever professionals, what are you looking for, these are my concerns, this is what I’m looking for, explain to me. And those meetings are always, usually very successful and very productive. Remember, you are your child’s best advocate, you know your child better than anybody else. And you have very good information which will help the therapist help your child.
[Anne] So make sure too, that please, if you have any questions, please put those in the Question and Answer chat so that we can take a look at those. So the other thing now, which I’m really glad that they’re doing this for many reasons, but the whole importance of cultural diversity. Cultural diversity, for many of us, we know as far as race, but it can also be a part of age, gender, sexual orientation, the ethnicity, and nationality, mental and physical ability. Knowing that a child who may have a physical disability, does not mean that that child also, they could be one of the smartest people you’ve ever met. It can also impact socioeconomic status and it can also impact religion. And so now, going forward, many of the colleges are placing into the curricula, training for new therapists, teaching them cultural competency and working with different families and working with different individuals. It’s very important for a therapist to understand a family’s culture and their beliefs and how that also works into the therapy plan. But it’s also very important for families to share that culture and beliefs with their therapists so that we’re not at cross purposes, but all working together.
For example we have, here at McMains, we have families that do not celebrate specific holidays, for some, Christmas, for different either religious views or their own personal things have chosen not to do that. So that’s important that when that child comes in, that that’s taken into consideration before we do a bunch of activities that are all centered around Christmas if it’s something that the family doesn’t want. English may not be the dominant language in a home. So a child may come in speaking English, the parent may speak English, but it’s important to know that the grandparents at home that also live with them only speak Spanish or only speak Chinese. And therefore you’d want to make sure that that’s taken into consideration so that a child who might (indistinct) different aspects of both languages are very important.
Another part of that is eye contact. Some cultures, eye contact means different things. And so it’s important to know that a child who may not be looking at you is not necessarily a sign of autism. It may not even be necessarily a sign of rudeness. It may be that in their family, in that cultural aspect, that that’s actually a sign of respect. And Medicaid does not mean poor. For socioeconomic status, Medicaid, as we all know, you can receive Medicaid many different ways. It is not just for a family who has a lower socioeconomic status, but it can also be through the Medicaid Waiver Program where those funds are waived. And Medicaid is a great resource to be able to carry on with therapy, especially on therapy services, because it covers therapy week after week. So it’s important that, okay, it’s important that Medicaid and Commercial Insurance or whatever that a child is seen as that individual and given the best care, no matter what that socioeconomic status is.
So in summary, a child may qualify for both School-based Therapy and Clinic-based Therapy. However, you may find that, sometimes, it may be only one of them. It could be, they could qualify for the Clinic-based and not the school therapy if they’re meeting all of their educational goals. We strongly encourage, learn the process. While upfront, sometimes that’s exhausting to know, have to learn one more thing. It is also very educating and strong, a strong advocating process for you that when you know what’s going on, it helps you be a better player in the game for all of us, including myself to know that process. Ask questions, don’t be afraid to question something. This is your child and you know your child best, and you are your child’s advocate. And lastly, communicate, communicate, communicate, we just can’t stress that enough. So thank you, and I guess we’ll move to the questions.
[Christina] Yes, at this time, we are gonna go to our questions, excuse me, our question and answer time. We did get a few questions while you guys were speaking. So I wanted to go over that. Let’s see here, the first question we have is, why would a child need speech therapy if they already talk, or if you have a young baby who would not be talking yet or any way?
[Anne speaking to Kim] That’s you, speech therapist [all laughing]
[Kim] Well, and that’s why it’s important to do an evaluation. Speech therapy is broken down to receptive language, which are the things that we’re understanding. And so maybe the child is not able to follow directions or, and then expressive are the things that we’re saying. So the child may be talking, but when they first start talking, they may put one word together, then two words together. If you have a four-year-old who is still only using one or two words, instead of three or four (indistinct) is not clear, and you cannot understand them, then you may want to seek help from a speech therapist. So it’s looking at, not only the things that they’re saying, but the things that they’re understanding as well. You know, are they beginning, especially young children, are they beginning to label pictures? If you say, “Oh, look, there’s a dog” and they know what you’re talking about, and are they understanding? “Oh, we’re looking, we’re fixing to go to grandma’s house.” Are they able to anticipate and know who grandma is? So it not only looks at the things a child says, but the things that a child is understanding as well.
[Christina] Great, thank you. Another question that was asked here is, If my child needs a service, but the school doesn’t agree, will I still be able to have insurance coverage for those services in the community?
[Anne] Yes, so remember the school is School-based Therapy. So there are things that a child may definitely, and the school may actually agree that they need it outside of school, but it’s not a problem in the classroom. So yes, you can go to a private care clinic and have your child evaluated for other options.
[Christina] Great, we have one more question here. It says, my five-year-old son has a form of cerebral palsy and gets OT at school. He loves the school speech therapist and his classroom teacher, but he does not like the OT. I don’t think she understands him. When I met with her, she said that he was a really difficult kid. I would like to get a different person to work with him. What could I do?
[Anne] Turn right to the social worker over here [all laughing]. So I think the first thing, maybe, it sounds like that she has tried, you have tried talking to the OT already and having that meeting and sometimes personalities just don’t match up, which is definitely, that’s okay. So I think the first thing, maybe to try with her again to ask, what are you trying, you’re saying that he’s difficult, is there something that he’s doing that maybe she’s able to help with, that you, as a mom can offer that well, he only does that when he gets really frustrated and maybe this is very frustrating for him. However, if that doesn’t help, then yes, you can request a different occupational therapist, who, hopefully, most schools will have more than one, who do come to that school. So I think that you can ask for that, but it may be something too, depending on where, if the occupational therapist is not really understanding that child, sometimes that’s a good place to start in helping to let them get to know each other a little bit better too.
[Christina] Okay, and then I’m assuming, it’s Ms. Fondal asked a question. It says, How do you continue therapies while out of school, like over summertime, when out of school and School Board states, a child does not require summer services.
[Anne] You can go to a private clinic and be evaluated through the clinic and get therapy that way. I mean, of course, School Board, all of that is based on what they see as the continuation if the child is going to have problems, to not receive it, you can ask, and again, appeal that process and try to find out if there’s anything that can be brought in along with that. But like I said, the other option is that you can go through a private clinic and get services and then start again in the Summer. [Christina] Great. [Kim] In the Fall. [Anne] The Fall, yes. ‘Cause it would be Summer.
[Christina] Right, now this was a very good question. I thought. It says, What if a child needs medical care in school, such as seizures or diabetes, but there’s no school nurse in the building?
[Kim] A lot of times what happens, and it depends on each individual school system and each individual school. I know sometimes they don’t have enough nurses to post a nurse at each individual school, but what they do is develop that health plan for that child. And so it may be another individual on that campus who has been trained by the school nurse or a doctor or family member or whatever, that has been trained. And in the health plan, they will step out. For example, if this child has a seizure, this is what happens and you do this and you do this and you do this, but they, a lot of times will have some. (audio cuts out)
[Christina] Well, we’re gonna hang out here for just a second and see if Anne and Kim come back on. Oh, there you guys are. Okay, we lost you guys there for a second. So excuse me, I’m gonna go to the last question we have here. And that is, My child is hard of hearing. The school wants her to have a FM system, so she can hear everything with her hearing aids, but I want her to have a teacher of the deaf. Do I have any options for getting her what I think is best for her?
[Anne] You wanna start? [Kim] I’ll start and Anne can jump in. Again, they’re looking (for) least restrictive environment. And so doing, doing what you can to make the child successful in school. And so that FM system becomes that accommodation to help the child and what they can do and the parent can watch is try that FM system and see if she is successful in that school setting. So that accommodation may be the tool that helps her, but if it is not, and she is still struggling to hear and still struggling to get the information in that you need. Then at that point is when you reconvene the IEP meeting and start talking about more intense instruction and perhaps a teacher for the deaf. And so I know they always try to start with the least interruptive, I guess, is a phrase to use right now and then work up. And so the simple accommodations and then working up to things that are more complex.
[Anne] No, I agree. And the FM, the system with that too, can follow her everywhere and is easier to be a part of that. Whereas the, not that someone signing would not be helpful, that just may not be available for every class where, for any other things that she’s doing. So it may also be something, again, to try the FM system. Now, as we’ve said, the whole way through, it is while we’re sitting down with that teacher and asking, as they’re developing that IEP, when it’s written in there, What’s the benefits of the FM system versus the benefits of having someone who can sign? And seeing if they have some other ideas as to what they’re thinking of, that maybe you have not thought of. There again, they may not be thinking of something that you have. And so sometimes just being told, well, we can’t afford that, is probably not the answer that it needs to be looked at and figured out from the overall process.
[Christina] Well, thank you guys for that. At this time we’re going to kind of transition into our transition, our discussion time, sorry. Anne and Kim will still be with us. But before we do that, I wanted to just let you guys know, excuse me, some of the webinars that we have coming up. Well, June 8th was yesterday, June 8th, we did the replay of last week’s webinar, which was “Preparing Your Child For Transition Into School.” Today’s June 9th, we’re doing, “Therapies And Accommodations.” We will be replaying this webinar with live discussion next week on Tuesday, June 15th. And then on June 16th, we will be doing a webinar with Maria Blanco about your child’s rights in special education. And then we will replay that, again, with the live discussion on June 22nd. Registration is open at /webinars. And we have posted a link in the chat for that. Let’s see, and then you can go to, I’m sorry, I got distracted, but you can go to that link and register for any of our webinars and the replays. Now, we’re gonna be going into our discussion time. At this point, we are gonna stop streaming and recording as we want anybody who’s present to feel comfortable discussing or asking questions, and having our talk. During the discussion time, you’re also gonna see a poll pop up and we ask that you complete that. Again, that’s just gonna kind of let us know how we’re doing and what else we can offer for you. We will be unmuting everybody during the discussion time. So we ask that you turn on your camera, if you’re with that and then unmute yourself and we can all talk. If you haven’t any tech problems during this time, again, you can send a message to the panelists through the chats. And at this time I’m going to let our. (audio ends)